Living with food allergies can feel daunting at times, whether it’s scanning labels in a hurry or nervously double-checking a restaurant order. But in Europe, we’re lucky to have strong systems in place, from clear food labelling to allergen-aware menus.
While it’s true that more individuals are being diagnosed with allergies, staying safe doesn’t have to mean living in fear. Whether you’re managing your own allergies or cooking for a friend, a bit of knowledge and a few smart habits can help you feel more confident about what’s on the dinner table.
First things first: What are food allergies?
A food allergy happens when your immune system overreacts to something that’s harmless for most people. You can be born with one, or it might show up unexpectedly later in life, even as an adult.1 Reactions usually happen within minutes of coming into contact with the food, and that contact can happen in a few different ways: by eating it, touching it, or even breathing in tiny particles.2
In rare cases, food-based ingredients in medications can also trigger a reaction. And it’s not just about the obvious stuff like peanuts sprinkled on a cupcake that people need to think about. Even a trace amount left behind from cross-contamination (also known as cross-contact) can be enough to trigger a response in people with severe allergies. For example, if someone slices a nut-based snack on a chopping board and you use it straight after without cleaning it properly, that could be enough to set off a reaction.3
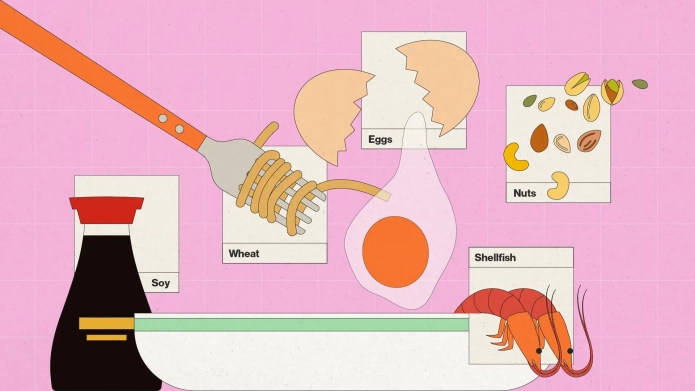
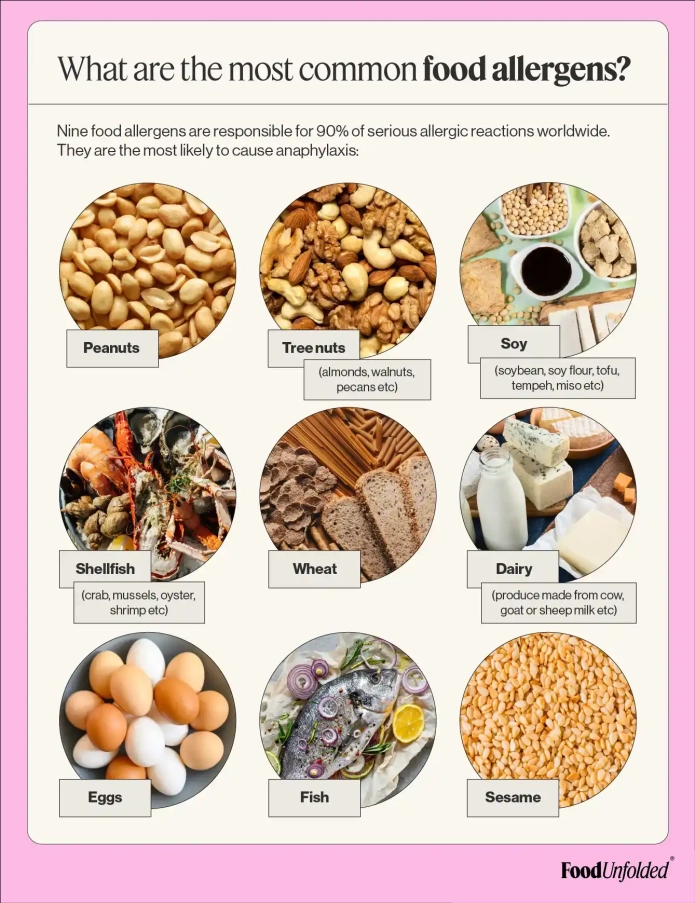
What are the most common food allergens?
When it comes to food allergies, a handful of ingredients are behind the vast majority of serious reactions worldwide. Nine common allergens are responsible for around 90% of them. You’ve probably heard of most — they’re the usual suspects on food labels and allergy warnings — but a few might surprise you:45678
- Peanuts
- Tree nuts (like hazelnuts, almonds, walnuts, cashews, and pecans)
- Milk and dairy (from cows, goats, or sheep — including butter, cheese, and yoghurt)
- Shellfish (such as crab, mussels, shrimp, and oysters)
- Fish
- Eggs
- Wheat
- Soy (including soybeans, tofu, soy flour, tempeh, miso, and more)
- Sesame (now officially recognised in many countries due to rising cases)
There are also a few rarer types of allergens that catch people off guard — like celery, mustard, or even kiwi fruit.
What happens if you eat a food allergen?
If you’re allergic to a food, your body might let you know in a few different ways — maybe with a rash, itchy skin, or swelling around your lips, face, or throat. Some people feel nauseous or get stomach cramps. Occasionally, allergies can even cause sneezing, though that’s more common with things like pollen.9
The most serious kind of reaction is called anaphylaxis. It can develop quickly and may include symptoms such as a swollen tongue or throat, wheezing, trouble breathing, dizziness or faintness, and a sudden drop in blood pressure. It’s rare, but it can be life-threatening, which is why it’s so important to be prepared.
Many people with severe allergies carry an epinephrine auto-injector (often called an EpiPen). This little device delivers adrenaline, which helps open up the airways, raise blood pressure, and calm the body’s reaction. They’re made to be simple to use — in fact, anyone nearby can step in and help. After using one, it’s important to call emergency services straight away.10
Did you know? Some of these symptoms, like a sore tummy or feeling unwell, can also be caused by food sensitivities or intolerances. These are not life-threatening, but they can still affect your health and wellbeing.11 1 12
The difference between food allergies and food sensitivities
Food allergies are one of the most common long-term health challenges in Europe, and for about 1 in 5 people with allergies, the symptoms can be severe enough to make everyday life pretty tough. Understandably, many people live with worry, fearing serious reactions like asthma attacks, anaphylaxis, or worse.13
But sometimes, what people think of as allergies might actually be food sensitivities. So, what’s the difference? Food sensitivities happen when your body has trouble digesting certain foods. Unlike allergies, the reaction usually shows up later and isn’t life-threatening.
With a food sensitivity (also called intolerance), many people can still enjoy a little bit of the food without trouble. But eating too much might lead to uncomfortable symptoms like bloating, gas, tummy aches, nausea, headaches or brain fog, tiredness, and even skin problems like eczema or itchy rashes.14
Knowing the difference can help you feel more in control and make smarter choices about what you eat, without unnecessary worry.
How can you test for food allergies?
If you think you might have a food allergy, it’s a good idea to see a doctor. They can help figure things out with tests like skin prick tests, blood tests, or sometimes supervised food challenges.15 We’re seeing more medically confirmed allergies these days, especially in kids, and while scientists have some ideas about why this might be happening, there’s still a lot we’re learning.
Why are allergies on the rise?
There are a few ideas: Spending more time indoors means less vitamin D from sunlight, which affects our immune system.16 The “hygiene hypothesis” suggests that being too clean might keep our immune system from developing fully.17 Family history plays a role too; kids with allergic parents have a higher chance of developing allergies, though not always to the same foods.18
Interestingly, delaying exposure to common allergens might actually increase allergy risk—early and repeated introduction can help the immune system learn to accept them.19 How we’re born also matters: babies born by C-section are more likely to have allergies, while breastfeeding can offer protection.20
Other factors like antibiotics, pollution, and diet may also affect allergies by causing inflammation in the body. It’s a complex puzzle, but understanding it helps us take better care of ourselves and our loved ones.
Who is responsible for managing food allergens?
It’s not just up to consumers with food allergies to protect themselves. If food labels didn’t include ingredients, how could people know whether they can eat it? People with allergies need help from the food industry, health professionals, and regulators such as the European Food Safety Authority (EFSA).
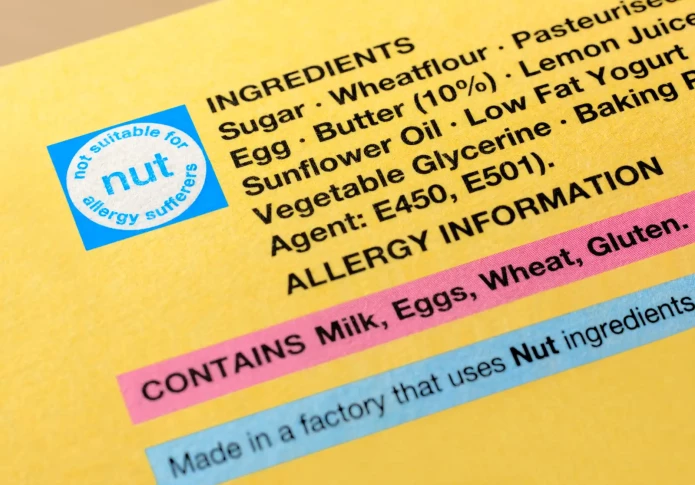
One of the most effective ways to protect people with allergies is by clearly declaring allergens on food packaging. But here’s the catch: this only works if producers know an allergen is in the product. Occasionally, allergens can easily sneak in through cross-contamination in production lines, shared storage areas, reusable equipment, human error, or even the cleaning process.
Take pasta, for example. A factory might make both egg-free and egg-based pasta using the same machines. If the equipment isn’t cleaned thoroughly between batches, tiny traces of egg could end up in the egg-free version. That’s why it's crucial to assess the risk of allergen contamination at every stage of food production, from ingredients and packaging to staff training and equipment cleaning.
To help manage this risk, many food producers use precautionary labelling. You’ve probably seen warnings like “may contain traces of nuts” or “made in a factory that also processes eggs.” These labels are used when there’s a small chance that allergens could be present, even if they aren’t actual ingredients.
How to avoid allergens
So now you have a better understanding of what allergies actually are, what steps can you take to avoid allergens?
1. Read food labels carefully.
In the EU, the main allergens (like milk, eggs, peanuts, gluten, soy, etc.) must be listed on the label of packaged foods. You can find them in bold, italics, or underlined in the ingredients list.21
2. Ask for the allergen menu.
Restaurants, cafés, and takeaways in the EU are legally required to provide allergen information. They might mark allergens on the main menu, on a separate allergen sheet, or tell you verbally.22 However, not all places always follow these rules, even though they should. To stay safe, always inform the person serving you about your allergy, ask them to note it in your order, and also verbally notify the chef.
Did you know? If you notice a restaurant isn’t providing proper allergen information, you can report it to your local food safety authority to help protect yourself and others.
3. Be cautious with unpackaged or homemade foods.
Market stalls, bakeries, and home-cooked meals may not have full labels and can carry a higher risk of cross-contamination. Make sure you talk to whoever is selling the food, and only go ahead if they can confirm that they know how to handle food allergens and exactly what’s in the food you buy.
4. Avoid buffet-style food and shared plates.
Serving spoons may be used for multiple dishes, increasing the risk of cross-contamination. If you have an allergy, it’s best to stick to your own plate rather than eating from platters with many different foods.
5. Check non-food products too.
Some cosmetics and medications can contain allergens, so always read the label. Ensure your doctor knows about your allergy and don’t hesitate to remind them before taking any new medications.
6. Be prepared when travelling.
Learn how to say your allergy in the local language, and consider carrying a card that explains your allergy clearly. Bring some snacks in your suitcase that you know you can safely eat in case it takes a while to find some safe food options abroad.
7. Carry emergency medication.
If you have one, always keep your Epi-Pen with you. Let your friends and family know where you keep it, e.g. in the side pocket of your backpack and how to use it. You could also consider wearing an allergy bracelet* so emergency services can quickly understand what’s wrong.
8. When in doubt, don’t eat it.
If you're not sure whether a food is safe, it's better to skip it than to take the risk.
*An allergy bracelet is a simple wristband that clearly tells others about your food allergies. Emergency services know to look out for them.
Hosting a friend with an allergy
If you’re reading this for someone you love, that shows how much you care. The best way to handle allergies is to prevent reactions before they happen. Here are some handy tips to help you cook safely and confidently for those you care about:
- Ask and remember: Double-check which foods to skip and how serious the allergy is.
- Keep it clean: Wash your hands, tools, and surfaces really well before you start.
- Use separate equipment: Keep allergen-free foods safe by using different knives and boards.
- Read those labels: Always check ingredients carefully. Look out for bold, italic, or underlined allergen words. Don’t forget to ask if the food might be listed under other names (for example, peanuts can sometimes be called arachides).
- Don’t mix it up: Keep allergen foods away from allergy-friendly ones to avoid any mix-ups.
- Tell the team: Make sure everyone at home knows about the allergies and what to watch out for.
- Label your dishes: Write down what’s safe and what’s not so no one gets confused.
- Be ready: Keep any allergy meds close by, just in case.
- Keep talking: Remind everyone to stick to the plan
Final thoughts
Living safely with allergies can feel worrying at times, especially when we hear about severe reactions in the news. Those stories are scary. But what often goes unnoticed are the countless calm, everyday moments when millions of people across Europe enjoy their meals, shop, and eat out without a single problem. Thanks to clear food labelling, allergy-friendly menus, and growing awareness, most people with allergies lead safe, full lives. And if a reaction does happen, tools like EpiPens and good healthcare are there to help in an emergency.
So yes, staying informed and careful is important—but we can also find peace in knowing we live in a world where an invisible safety net is built around our daily routine.
References
- European Food Safety Authority. (n.d.). Food allergens. Retrieved May 8, 2025, from
- Sicherer, S. H., & Sampson, H. A. (2014). Food allergy: Epidemiology, pathogenesis, diagnosis, and treatment. Journal of Allergy and Clinical Immunology, 133(2), 291–307.e5.
- United States Food and Drug Administration. (2021). Food allergens.
- Nwaru, B. I., Hickstein, L., Panesar, S. S., Roberts, G., Muraro, A., Sheikh, A., & the EAACI Food Allergy and Anaphylaxis Guidelines Group. (2022). Frequency of food allergy in Europe: A systematic review and meta-analysis. Allergy, 77(3), 816–829.
- Lyons, S. A., Clausen, M., Knulst, A. C., Burney, P., & Dubakiene, R. (2020). Prevalence of food sensitization and food allergy in European children: EuroPrevall birth cohort. Allergy, 75(11), 2867–2878.
- NHS. (2023, January 5). Food allergy. NHS. Retrieved July 2, 2025, from
- NHS. (2023, June 21). Anaphylaxis. NHS. Retrieved July 2, 2025, from
- Cleveland Clinic. (2025, April 1). Allergies: Types, symptoms, treatment & management.
- NHS. (2022, November 25). Food intolerance. NHS. Retrieved July 2, 2025, from
- Allergy UK. (n.d.). Statistics and figures. Accessed 16th May 2025
- Cleveland Clinic. (2021). Food intolerance: Symptoms, causes and treatment options.
- National Library of Medicine. (n.d.). Food allergy testing. MedlinePlus. Accessed 16th May 2025.
- Mirzakhani, H., Al‑Garawi, A., Weiss, S. T., & Litonjua, A. A. (2015). Vitamin D and the development of allergic disease: How important is it? Clinical & Experimental Allergy, 45(1), 114–125.
- Perkin, M. R., & Strachan, D. P. (2022, November 24). The hygiene hypothesis for allergy – conception and evolution. Frontiers in Allergy, 3, Article 1051368.
- Koplin, J. J., Allen, K. J., Gurrin, L. C., Peters, R. L., Lowe, A. J., Tang, M. L. K., & Dharmage, S. C. (2013). The impact of family history of allergy on risk of food allergy: A population-based study of infants. International Journal of Environmental R
- Abrams, E. M., Ben-Shoshan, M., Protudjer, J. L. P., Lavine, E., & Chan, E. S. (2023). Early introduction is not enough: CSACI statement on the importance of ongoing regular ingestion as a means of food allergy prevention. Allergy, Asthma & Clinical Immuno
- American Academy of Allergy, Asthma & Immunology. (2024, June 20). Cesarean delivery increases risks of asthma and allergies in offspring. The Journal of Allergy and Clinical Immunology: In Practice. Retrieved July 2, 2025, from
- European Commission. (n.d.). Food labelling – general EU rules. Your Europe. Retrieved July 2, 2025, from
- European Parliament & Council of the European Union. (2011). Regulation (EU) No 1169/2011 on the provision of food information to consumers. Official Journal of the European Union, L 304, 18–63.
Do you care about thefood system?
Take part in our Annual Survey 2025
Take the survey